DEPARTMENT OF MAXILLOFACIAL SURGERY
HOSPITAL UNIVERSITARIO DE "LA PRINCESA "
MADRID (SPAIN)
Head : Dr. Diaz Gonzalez
ARTHROSCOPIC DISC SUTURING: CLINICAL RESULTS
Sastre J. ; Rodriguez Campo F.J. ; Gil-Diez J.L. ; Muņoz M. ; Ortiz de Artiņano F. ; Naval L. ; Padron A. ; Rubio P. ; Diaz Gonzalez F.
Introduction: About 20 % of people today have symptoms of temporomandibular joint (TMJ) dysfunction and an additional 50 % have one or both of their articular discs displaced but remain asymptomatic. Of these, it is estimated that about 5% will have symptoms severe enough to cause them to seek treatment.(1)
Purpose: The aim of this study is to evaluate the clinical results of patients with TMJ derangement treated by arthroscopic disc suturing and to compare this group versus other Wilkes stage (IV) group treated by lysis and lavage.
Material and Methods: Between March 1995 and September 1997, 101 patients were treated for internal derangement of the TMJ by arthroscopic surgery. This study included 16 patients (3 Wilkes III and 13 Wilkes IV) in the disc suturing group and 59 (Wilkes IV) in the lysis and lavage group. In all patients TMJ arthroscopy was performed after conservative treatment faillure. Surgical technique (2, 3) was performed under general anesthesia, intra-articular lavage was made with Ringer`s lactate solution and PDS suture was used to disc fixation. Postoperative treatment included: pharmacotherapy, soft diet, occlusal splint, and physiotherapy. Preoperative and postoperative evaluations were done at 1 month, 3 months, 6 months, 9 months and 1 year. This included determination of interincisal opening, protrusive movement and joint pain (Visual Analogic Scale -VAS- 0 to 100 mm ). The outcome of disc suturing group and comparation of the long term results of Wilkes IV group treated by disc suturing vs lysis lavage were made. Wilcoxon test was used to compare mouth opening of the two groups at each time point, and the amount of pain in the TMJ at each stage. Statistical significance was claimed for p< .05.
DISC SUTURING TECHNIQUE (2), (3).
..........................................1...............................................2..................................................3


1. Anterior disc displacement without reduction. Posterior ligament (LP) under the temporal eminentia (E). Roofing 0-25%.
2. Release of the anterolateral capsule with McCain scissors.
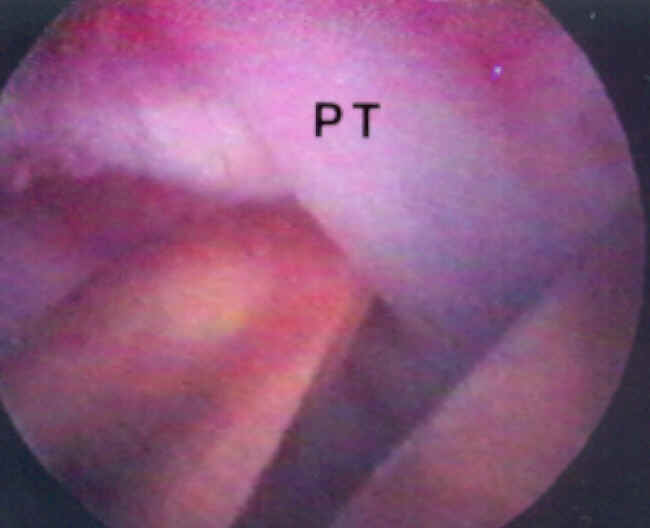
3. Lateral Pterygoid muscle (PT) is been cut with McCain scissors.
.............................................................4..............................................................5
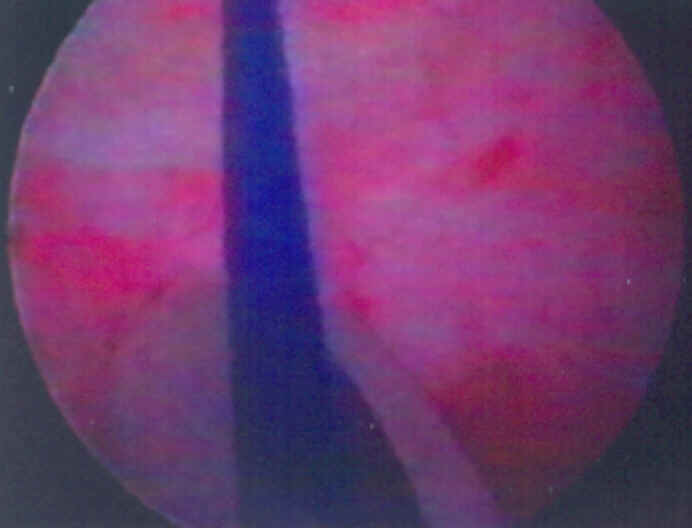
4. PDS suture in the posterior recess.
5. Alligator forceps is used to take out the suture.
RESULTS
Patients Characteristics
| ..Lysis-Lavage.... | ..Disc Suturing.... | |
| ....Nš Patients | ......85 | ......16 |
| ....Wilkes III | ......26 | ......3 |
| ....Wilkes IV | ......59 | ......13 |
| ....Nš Joint ........Bilat. ........Unilat. |
......106 ......21 ......64 |
......21 ......5 ......11 |
| ....Age ....Male ....Female |
......27.6 years ......10.6% ......89.6% |
......24.5 years ......13% ......87% |
Patients History
| ....Lysis-Lavage.... | ....Disk Suturing.... | |
| ....No History | .......27 | .......6 |
| ....Trauma | .......8 | .......0 |
| ....Bruxism | ......16 | .......8 |
| ....Orthodontic .Treatment. | ......4 | .......0 |
| ....Arthrocentesis ....Others |
......1 ......2 |
.......0 .......2 |
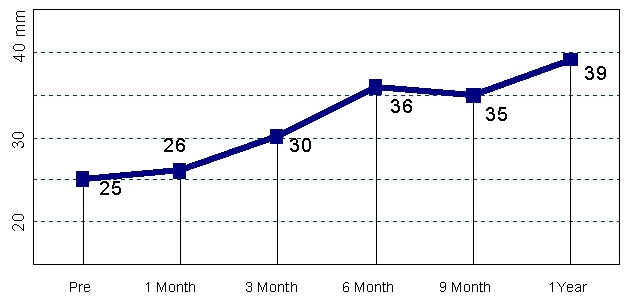
MOUTH OPENING ( Disc Suturing Group) N=16
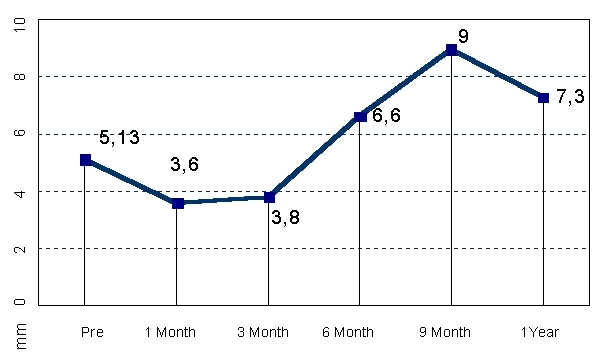
PAIN (Disc Suturing Group) N=16

PROTRUSIVE (Disc Suturing Group) N=16
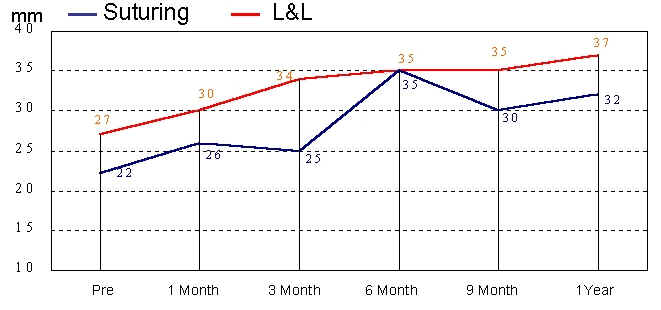
PAIN Wilkes IV (SUTURING vs L&L) (13 vs 59)
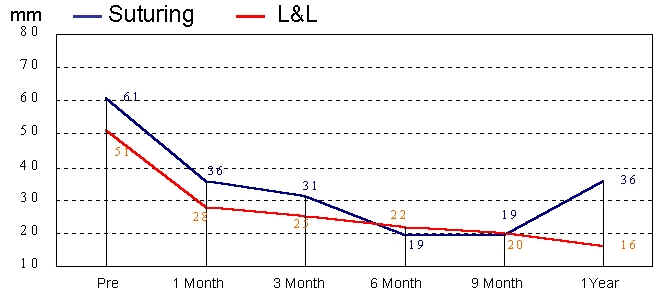
MOUTH OPENING Wilkes IV (SUTURING vs L&L) (13 vs 59)
DISCUSSION
The results of this study demostrate that the arthroscopic disc suturing is an effective surgical technique for treatment of TMJ internal derangement secondary to anteromedial disk displacement without reduction. The follow up reveals an improvement of pain and dysfunction of the TMJ. The differences between lysis-lavage and disc suturing groups were not significant. This procedure has been applied by McCain, reporting an 82% of discal repositioning (2). In the present study MRI was not performed to evaluate discal repositioning. A correlation between disc position and TMJ osteoarthrosis has been described by Leeuw (4). In accordance with these reports, the normal disc position decrease the incidence of osseos changes in the long term follow up. However the procedure is technicaly difficult and it should be performed by a surgical team with advanced experience in arthroscopic procedures. Only prospective, randomized and controlled studies could eventually clarify the effectiveness of arthroscopic disc suturing for the discal reposition.
CONCLUSIONS
1. The arthroscopic disc suturing improves pain and dysfunction in patients with internal derangement of TMJ.
2. In the Wilkes IV stage, the clinical results were similar in both groups.
3. Although the arthroscopic disc suturing is technically difficult, the rate of complications was similar to the lysis-lavage group.
References:
1. http://copland.udel.edu/~kristym/anatomy.html
2. McCain J.; Podrasky A.E.; Zabiegalski A. Arthroscopic disc repositioning and suturing: a preliminary report. J. Oral Maxillofac Surg 50:556-579.1992.
3. Israel H.A. Technique for pacement of a discal traction suture during temporomandibular joint arthroscopy. J. Oral Maxillofac Sur 47:311-313.1989.
4. Leeuw R.; Boering G.: Van der Kuijl B.; Stegenga B. Hard and soft tissue imagin of the temporomandibular joint 30 years after diagnosis of osteoarthosis and internal derangement. J Oral Maxillofac Surg 54:1270.1996